
LCS 3 Fort Worth launched in December 2010 at Marinette Marine Corp. (MMC) of Fincantieri Marine Group. In May, MMC held a ribbon-cutting ceremony to commemorate the opening of the company’s newest facility, and to mark the completion of Fincantieri’s $73-million investment in the shipyard in Marinette, Wis. The company’s proactive approach to its employees’ health care has helped it keep premiums under control while hiring hundreds more people.
For any company that plans to open a new facility, or expand an existing one, the decision must make financial sense. In most cases, the two biggest concerns are quality of the work force and the cost of that work force (wages and benefits). Plenty of states have high-quality work forces. That means the decision on where to locate often comes down to the cost of labor — and health care is a huge part of that cost.
Health care costs increase about 10-12 percent every year. HR directors expect that to jump to 12-15 percent in 2014 when the Affordable Care Act kicks in, which makes reducing health care costs that much more imperative.
Many companies tend to focus on the up-front cost of health care — what will it cost this year? Where can they find the lowest premiums? The problem with this perspective is that health care is viewed as an expense, instead of an investment. A different approach would be: What will our health care costs be three, five, or 10 years from now? How can we deliver the highest quality of care at the lowest possible cost? How can we leverage a healthy and happy work force to improve our bottom line?
What many businesses don’t realize is that access to high-quality health care will reduce health care costs over time — sometimes by as much as 40 to 50 percent — with subsequent premium increases far below the national average. Of course, this has a dramatic impact on the financial performance of the company, as well as on the productivity and contentment of its employees.
Look no further than Wisconsin to find one of the top states in the U.S. for high-quality health care. Its high ranking is the result of a proactive and collaborative culture where state agencies and organizations, health-care systems, payer systems and employers work together to develop innovative solutions that deliver highly effective and efficient care, as well as reduce costs. And Wisconsin is well ahead of the curve when it comes to innovation — the state began its own health-care “reform” initiatives a decade before the Obama Administration enacted the Affordable Care Act in 2010.
“ Collaborations among employers, providers and payers push everyone to be more innovative and transparent, which creates a competitive advantage for the state.“
— John Torinus, CEO, Serigraph

For example, Serigraph, a printing, molding, and custom graphics company in West Bend, collaborated with health providers to create a consumer-oriented approach to health care that has greatly improved employee health and reduced health care costs. The company’s annual cost per employee is $9,000, about 40 percent below the national average of $15,000 per year.
In giving talks across the country on the Serigraph model, CEO John Torinus has noticed many states are far behind when it comes to health-care innovation.
“There is no doubt Wisconsin is a health-care leader in both the public and private sectors,” he says. “Collaborations among employers, providers and payers push everyone to be more innovative and transparent, which creates a competitive advantage for the state.”
This collaborative spirit also led to the formation of the Wisconsin Health Information Organization (health-care providers, health insurers and employer representatives working together on payment reform) and the Wisconsin Hospital Association’s (WHA) Price Point wiPricePoint.org and Check Point wiCheckPoint.org initiatives. Wisconsin was one of the first states to provide hospital prices online to the public. WHA’s PricePoint.org is one of the best sources of hospital price information in the nation and is used in 14 states.
The Wisconsin Difference
Many states have yet to restructure their approach to health care, which typically takes at least five years to mature to the point where big improvements can be made. Wisconsin has been improving its health-care programs for two decades, and has the results to prove it:
- Most of Wisconsin’s health-care organizations have adopted evidence-based care pathways and guidelines – as a result, Wisconsin’s efficiency index of 0.94 (cost for care of a Medicare patient) ranks 12th in the nation.
- Wisconsin ranked second only to Minnesota in overall health-care quality scores based on 171 measures by the federal Agency for Healthcare Research and Quality (AHRQ). Other states that did well include Maine, Massachusetts and Iowa.
- The average health care spending index at individual hospitals in Wisconsin is between .86 and .96, well below the national average (Kaiser Health Care News, May 2012).
- According to a 2012 Commonwealth Fund Report on local health system performance, several Wisconsin communities placed in the top 10 in the country, and every Wisconsin community ranked in the top 25 percent.
- A 2013 Commonwealth Fund Report that ranked overall health system performance for low-income populations placed Wisconsin among 12 states that ranked in the upper quartile. The report noted that “Healthier adults are less expensive to care for and have greater work-force productivity; healthier children are more likely to succeed in school and grow up to continue to participate in the work force in the future. A healthy population is thus instrumental in maintaining strong local and state economies, as well as the nation’s economic health and well-being.”
These enviable rankings are a result of the many ways Wisconsin health systems have worked to increase quality and reduce cost. When patients have quick access to excellent care and are rapidly assessed, efficiently diagnosed, and well-managed, their care is less expensive, especially over time. They also miss less work because of illness or disability. This type of coordinated, streamlined care is also facilitated by highly integrated medical centers.

Dr. Timothy Johnson is president and CEO of Mayo Clinic Health System in La Crosse, Wis.
“Chronic disease is responsible for much of the cost for health care,” says Dr. Timothy Johnson, president and CEO of Mayo Clinic Health System in La Crosse, Wis. “These costs can be managed only by aggressively coordinating the care of the patients. There are many examples of patient-centered medical homes and care-coordination models that are improving care while lowering the cost for these challenging patients.”
Wisconsin health-care systems work directly with employers and employer groups to lower costs and improve access, while maintaining the quality that employers and employees have come to expect. Many integrated delivery systems have been operating as accountable care organizations (ACOs) for years, with aligned incentives that work well for both providers and payers.
Integration and Communication
Integration and connectivity are absolutely essential for optimizing care and holding down costs.
“In general, health care in Wisconsin is much more connected compared to most states, and stunningly better than others,” says Dr. Jeffrey Thompson, CEO for Gundersen Health System in La Crosse.
Multiple layers of connectivity include electronic health records, best practice protocols, shared education programs, electronic fetal monitoring sites and emergency room telemedicine in real time.
Gundersen Health System has invested heavily in primary care, disease management, and rehabilitation. Nurses and social workers collaborate with multiple providers to coordinate services and resources across the continuum of health care. This care coordination program works with patients of all ages and is a service provided at no cost to patients.
“By spending $1 million to proactively manage the health care of the sickest 1 percent of the work-force population, we save $10 million in hospitalization costs every year,” says Thompson. “This keeps rate increases at about 4 percent, well below the 12-15 percent national average.”
On the other side of the state, Milwaukee was recently cited as being one of only three cities nationwide that has both below-average treatment costs and above-average quality, according to an analysis conducted by HCTrends and The Benefit Services Group. The study compared health-care costs in 24 urban areas using a cost-per-episode approach. It found that Milwaukee providers are among the most efficient in treating diabetes, obesity, migraine headaches and depression.
Milwaukee was recently cited as being one of only three cities nationwide that has both below-average treatment costs and above-average quality.
An earlier study released in 2012 found that hospitals in southeastern Wisconsin on average were controlling costs better than their counterparts throughout the country and that health insurance premiums here were rising at a slower rate than the Midwest and national averages.
“Rural or urban, Wisconsin health-care providers are focused on reducing health-care costs through coordination of services and a patient-centric model of care,” according to Wisconsin Hospital Association Executive Vice President Eric Borgerding. “For many of our health-care systems, their knowledge on how to lower employee health-care costs comes from their experience and innovations they have applied in their own work environment.”
Aurora Health Care’s integrated approach to health care has dramatically reduced the cost of its employee health plan. Between 2001 and 2010 Aurora significantly outperformed the national trend, posting an average increase of 6.2 percent per year, compared to 10.7 percent per year for preferred provider organizations (PPOs) nationally.
“As a result of this differential,” says Peter Garner, director of ACO consulting for The Benefit Services Group, “Aurora’s per-member, per-month costs are 42 percent lower than they would have been if they had increased at the national average for non-integrated networks.”

“We are taking our commitment to promoting a culture of improved health and wellness within our company to the next level.“
— Kerry Arent, senior vice president of human resources, Appleton Papers
Another innovative leader that is achieving impressive results is Bellin Health in Green Bay. As reported in The New York Times, The Foth Companies, an engineering and consulting firm, has worked with Bellin Health to keep its medical premium increases at least 50 percent below the national average for five of the last six years. Another Bellin customer, Northeast Wisconsin Technical College, had no premium increase per employee in 2012 and does not expect one in 2013. Fincantieri Marine Group, which builds ships at its facility in Marinette, has been able to increase its work force by 600 people and still keep health care premiums under control for the last several years.
“We partnered with Bellin Health because they have the same philosophy we do,” says Steve Baue, vice president of human resources, Marinette Marine Corp. “As a corporation we look at bottom-line dollars. But there are so many returns on investment that come with this proactive approach that are impossible to quantify.”
An Investment, Not an Expense
The health care field is rapidly evolving and, with the passage of the ACA, has never been more complex. It is therefore critical for companies to innovate and be proactive to stay ahead of the curve. This will be far more difficult to achieve in a state that does not have a track record of innovation and high-quality care.
Quality does cost more up front – but it also lasts longer. Wisconsin does not have the least expensive health care — in fact, average family insurance premium costs are higher than the national average, as are health-care expenditures per capita. However, the higher quality of health care in Wisconsin translates into happier and more productive employees, higher quality of life, better retention, and overall lower health care costs, especially over time as employees become healthier.
Fincantieri Marine Group, which builds ships at its facility in Marinette, has been able to increase its work force by 600 people and still keep health care premiums under control for the last several years.
Using 2011 data from the Agency for Healthcare Research and Quality, the average premium in Wisconsin for a family is about $12,200; the lowest premiums in other states averaged about $9,200 per family per year. Locating in one of these lowest-cost states saves a company about $3,000 per employee per year compared to Wisconsin. However, a company in Wisconsin can take full advantage of the innovative health care programs in the state and knock its premium costs down by 30 percent or more, reducing the premium to about $8,500 or less per employee per year – a significant savings over the lowest-cost states. Further, the probability is high that premiums in the lowest-cost states will continue to rise at double-digit rates, while increases for innovative health care in Wisconsin will be lower, or even flat.
Then there is the huge impact of better health-care results.
According to the 2011 AHRQ Quality Map for “Health Care Quality Comparison of All States,” Wisconsin’s overall health care is ranked “strong,” while the lowest-premium states are ranked “weak.” One reason Wisconsin is “strong” is because it has been so effective in actively managing chronic disease conditions such as diabetes, high blood pressure, and obesity – thereby improving health, reducing complications, and keeping employees out of hospitals and other high-cost situations. According to the Centers for Disease Control, chronic diseases contribute to 75 percent of all health-care costs. The lesser ability to control these diseases in the weakest states will drive up premium costs significantly over time.
Providing outstanding health care also leads to higher employee satisfaction. Healthier workers are happier, more productive and feel more valued. Absenteeism is lower. This is one reason why Appleton Papers partnered with ThedaCare in Appleton to improve employee wellness.
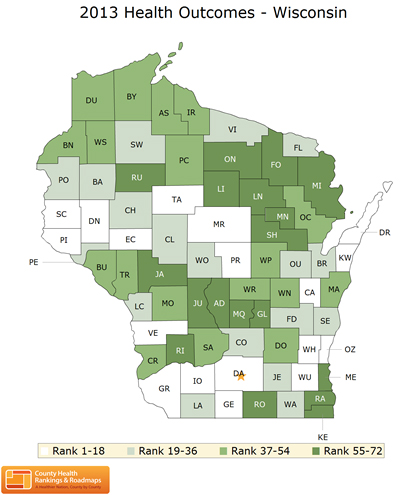
Water Views: The University of Wisconsin Population Health Institute, along with the Robert Wood Johnson Foundation, in March released the 10th edition of health rankings in Wisconsin. Wisconsin’s five healthiest counties are Ozaukee, Kewaunee, St. Croix, Pierce, and Door, all of which are located on either Lake Michigan or the Mississippi River.
“We are taking our commitment to promoting a culture of improved health and wellness within our company to the next level,” says Kerry Arent, senior vice president of human resources for Appleton Papers. “Healthy employees have a better quality of life, are more engaged, and work more safely. Improved health and wellness can help lower health-care costs for employees and our company – a scenario where we win together.”
Wisconsin is one of the most experienced states in the country when it comes to providing innovative, high-quality health programs. After nearly two decades of improvement, this culture is solidly in place and other states look to Wisconsin for leadership. A proven track record is extremely important to CEOs, especially when steady gains can be seen over time and continue through major upheavals, like recessions and elections. CEOs also like to see evidence of reinvestment and continual improvement. Wisconsin provides all this and more.
Long-term collaborations among the Wisconsin Department of Health Services, Wisconsin Hospital Association, hospitals, providers, payers, and private-sector companies have resulted in nation-leading improvements in the quality and efficiency of health care – resulting in reduced or even flat cost increases. Because Wisconsin provides some of the best health care in the nation, companies that locate within the state will be provide their employees with outstanding health care at competitive rates, enjoy lower-than-average premium increases in the future, and improve worker productivity and satisfaction.
Mary Kay Grasmick is vice president of communications at the Wisconsin Hospital Association, located in Madison.