Looking for motivation for that New Year’s fitness commitment? Looking for a healthy populace from which to hire? New reports on obesity and heart attack incidence could be your guides for both.
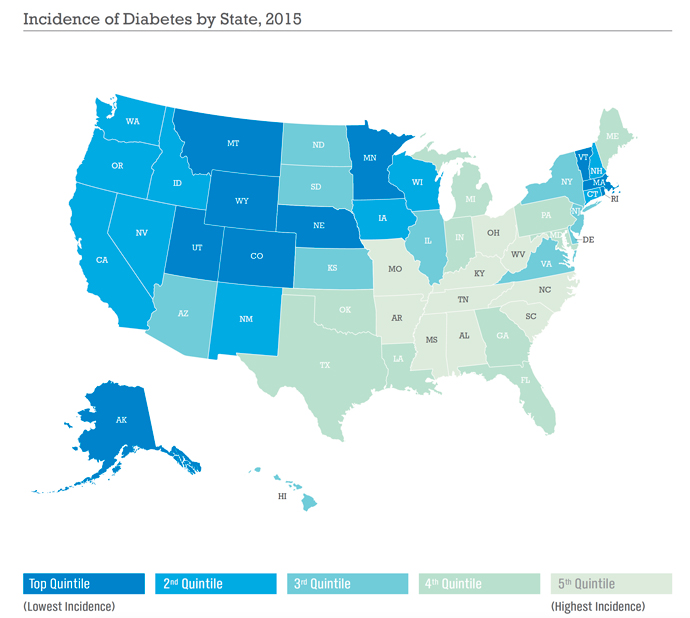
As part of their State of American Well-Being series, Gallup and Healthways in November released their 2015 State and Community Rankings for Incidence of Diabetes report, ranking 190 metro areas as well as the 50 states.
“Since Gallup and Healthways began tracking this metric in 2008, an estimated 2.2 million more adults report that they have been diagnosed with the disease,” said the organizations, noting the nation’s 11.5-percent diabetes incidence rate, “while the obesity rate, a significant risk factor for the development of diabetes, has climbed by almost three points since 2008, to reach 28.3 percent nationally in 2016.”
Incidence of Diabetes in States Across the U.S.
Lowest Incidence
| 1 | Utah | 7.40% |
| 2 | Rhode Island | 7.60% |
| 3 | Colorado | 7.90% |
| 4 | Minnesota | 8.40% |
| 5 | Montana | 8.70% |
| 6 | Alaska | 8.80% |
| 7 | Massachusetts | 8.90% |
| 8 | Vermont | 8.90% |
| 9 | Nebraska | 9.10% |
| 10 | Wyoming | 9.30% |
Highest Incidence
| 41 | North Carolina | 13.50% |
| 42 | Missouri | 13.50% |
| 43 | Ohio | 13.50% |
| 44 | Kentucky | 13.70% |
| 45 | Arkansas | 14.10% |
| 46 | South Carolina | 14.40% |
| 47 | Tennessee | 14.40% |
| 48 | Mississippi | 15.60% |
| 49 | West Virginia | 16.10% |
| 50 | Alabama | 16.10% |
The analysis measures prevalence of the disease by asking individuals if they have ever in their lifetime been diagnosed with diabetes. The state ranking is based on a subset of 176,885 telephone interviews with US adults across all 50 states, while the community ranking is based on 246,620 interviews. Utah, Rhode Island and Colorado have the lowest incidence of diabetes in the nation, with less than 8 percent of their adult populations having been diagnosed with the disease. Alabama and West Virginia have the highest diabetes prevalence, both with more than 16 percent of their residents diagnosed with diabetes.
Boulder, Colorado; Bellingham, Washington; Fort Collins, Colorado; and Provo-Orem, Utah, are the communities with the lowest prevalence of diabetes. No wonder it seems like Mountain Time means healthy time.
“Boulder distinguishes itself as the only community in the Gallup-Healthways rankings with less than five percent of its population reporting having been diagnosed,” said a release. “Residents of Mobile, Alabama and Charleston, West Virginia, report the highest rates in the nation, with more than 17 percent of their respective adult populations having the disease.
Incidence of Diabetes in Communities Across the U.S.
Lowest Incidence
| 1 | Boulder, CO | 4.90% |
| 2 | Bellingham, WA | 6.10% |
| 3 | Fort Collins, CO | 6.50% |
| 4 | Provo-Orem, UT | 6.50% |
| 5 | Cedar Rapids, IA | 7.30% |
| 6 | Salinas, CA | 7.40% |
| 7 | Ann Arbor, MI | 7.40% |
| 8 | Anchorage, AK | 7.70% |
| 9 | Amarillo, TX | 7.80% |
| 10 | Bridgeport-Stamford, CT | 8.00% |
Highest Incidence
| 181 | McAllen-Edinburg-Mission, TX | 15.70% |
| 182 | Beaumont-Port Arthur, TX | 15.80% |
| 183 | Rockford, IL | 16% |
| 184 | Flint, MI | 16.30% |
| 185 | Columbus, GA-AL | 16.40% |
| 186 | Little Rock-Conway, AR | 16.50% |
| 187 | Hickory-Lenoir-Morganton, NC | 16.80% |
| 188 | Corpus Christi, TX | 16.90% |
| 189 | Charleston, WV | 17.60% |
| 190 | Mobile, AL | 17.70% |
Obesity, commonly defined as having a Body Mass Index (BMI) of 30 kg/m2 or greater, is a significant risk factor for the development of type 2 diabetes. Other risk factors include age, physical inactivity, race and ethnicity, and genetic predisposition. How do you calculate obesity? By looking at the international standard followed by the World Health Organization: the body mass index, or BMI. It’s a person’s weight divided by the square of his or her height. As the Milken report and the NIH’s own BMI calculator define things, here are the cutoffs:
- Underweight: below 18.5
- Normal: 18.5 to 24.9
- Overweight: 25 to 29.9
- Obesity: 30 or higher
The U.S. standards follow the WHO’s and, tellingly, include a classification of extreme obesity, indicated by a BMI of 40 or higher.
Toxic Mix Calls for Blended Solutions
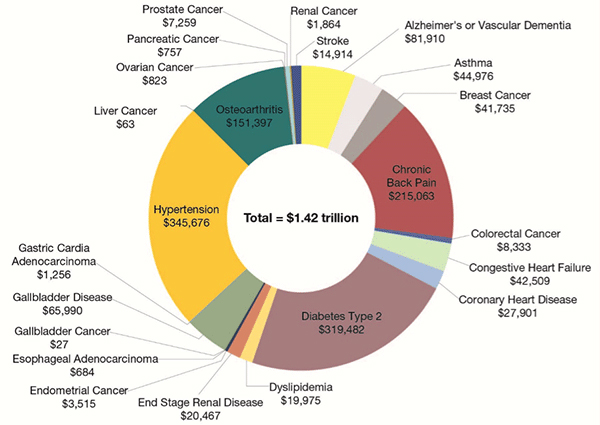
The coincidental Milken Institute report seeks to document the price of obesity, and declares that the “total cost to treat health conditions related to obesity — ranging from diabetes to Alzheimer’s — plus obesity’s drag on attendance and productivity at work exceeds $1.4 trillion annually. That’s more than twice what the US spends on national defense. The total, from 2014 data, was equivalent to 8.2 percent of US GDP, and it exceeds the economies of all but three US states and all but 10 countries.”
In 2014, 98.7 million US residents had obesity, and another 89.9 million were overweight, Milken says. If the obesity epidemic is not stopped and reversed, says the report, “the first generation of Americans born after the baby boomers (Generation X) could be the first to see its life expectancy decline, undoing many of the benefits that improving health status bestowed on our economy in the 20th century.”
Why has it occurred? Affordable bad food in big portions, and less physical activity as the services economy and leisure time filled with electronics means a work day and play time alike that overload the brain but ignore the rest of the body. Milken turns to its technology expertise for the metaphor: “According to the first law of thermodynamics, energy cannot be created or destroyed. In the context of obesity, the human body expresses that principle by converting energy to fat for use at another time.”
Where do other nations stand? As recently as 2013, Mexico was just behind the US with obesity at 32.4 percent. “New Zealand, Hungary, Australia, Canada, Chile, the UK, and Ireland were not far behind. East Asian nations such as Japan and South Korea had the lowest obesity rates at 3.6 percent and 4.6 percent, respectively,” says the report. “However, pre-obesity rates in these nations are growing at substantially faster paces, suggesting that the obesity epidemic and its associated conditions may be coming to their shores.”
In 2014, the direct costs of medical treatment for health conditions causally related to obesity and overweight totaled $427.8 billion in the US. Among those conditions, type 2 diabetes had the highest treatment costs, at $111.9 billion. Alzheimer’s disease and vascular dementia were next, with $56 billion in direct treatment costs. Gallbladder disease was next with $43.9 billion, followed by osteoarthritis at $42.1 billion.

However, said Milken, a review of interventions designed to reduce obesity concluded that for individuals with a body mass index (BMI) of 40 or greater, “a 5-percent weight reduction would yield $2,137 in medical cost savings annually. For individuals with a BMI of 35, the same percentage reduction would result in $528 savings.”
“We see a great need for a multifaceted, long-term commitment to advocating for healthy body weight,” the report concluded, including a call for an anti-obesity campaign similar to the anti-smoking ads of the 1970s. “Employers, medical providers, insurers, biopharmaceutical firms, the food and beverage industry, governments, and communities must work together — and the individuals affected by obesity and being overweight need to accept some personal responsibility to modify their behavior.”
A separate report in the Well-Being Index series from Gallup-Healthways ranks communities by incidence of heart attack. Again, being in the mountains or in a college town seems to help.
Boulder and Ann Arbor have the lowest incidence of adults who have experienced a heart attack during their lifetime, each with 1.3 percent.
“Both communities have consistently demonstrated high well-being as measured by the Gallup-Healthways Well-Being Index since 2008, as well as low incidence of other chronic conditions such as high blood pressure, high cholesterol, and diabetes,” said the report. “Tallahassee, Provo, Austin, and San Jose are the other top metros, each with less than a 2.0-percent incidence of heart attack,” closely followed by two more California communities, the hometown of the University of Florida (Gainesville) and, amazingly enough for you stereotypers out there, the cheesehead capital of the world — Green Bay, Wisconsin — with an incidence of just 2.2 percent.
“At the other end of our rankings, eight communities have more than 7 percent of residents who have experienced a heart attack,” said the report. That means you, Charleston, West Virginia; Deltona-Daytona Beach-Ormond Beach, Florida; Duluth, Minnesota-Wisconsin; Huntington-Ashland, West Virginia-Kentucky-Ohio; Youngstown-Warren-Boardman, Ohio-Pennsylvania; Lake Havasu City-Kingman, Arizona; Chico, California; and Fort Smith, Arkansas-Oklahoma.
The report points to the growing field of lifestyle medicine — exemplified by the Ornish program — as one possible solution to improved heart and overall health.
Ways Forward?
What might this have to do with corporate location decision-making? Well, just as companies look for other kinds of infrastructure to undergird their sites — water, transit and highways, electrical power, broadband — they might look more closely at the infrastructure of an active lifestyle. A Gallup-Healthways report authored by Dan Witters and nader Nekvasil issued earlier this fall offers some guidance.
Gallup and Healthways created an Active Living Score for 48 medium to large MSAs by analyzing metropolitan infrastructure data — including walkability, bike-ability, transit infrastructure and park infrastructure — based on each community’s Walkscore® and ParkScore®.
Top and Bottom 10 Communities for Incidents of Heart Attack
Top 10 Communities
| 1 | Boulder, CO | 1.30% |
| 2 | Ann Arbor, MI | 1.30% |
| 3 | Tallahassee, FL | 1.50% |
| 4 | Provo-Orem, UT | 1.60% |
| 5 | Austin-Round Rock, TX | 1.80% |
| 6 | San Jose-Sunnyvale-Santa Clara, CA | 1.90% |
| 7 | Visalia-Porterville, CA | 2.00% |
| 8 | San Luis Obispo-Paso Robles-Arroyo Grande, CA | 2.10% |
| 9 | Gainesville, FL | 2.10% |
| 10 | Green Bay, WI | 2.20% |
Bottom 10 Communities
| 181 | Kingsport-Bristol-Bristol, TN-VA | 6.80% |
| 182 | North Port-Sarasota-Bradenton, FL | 7.00% |
| 183 | Fort Smith, AR-OK | 7.10% |
| 184 | Chico, CA | 7.10% |
| 185 | Lake Havasu City-Kingman, AZ | 7.20% |
| 186 | Youngstown-Warren-Boardman, OH-PA | 7.40% |
| 187 | Huntington-Ashland, WV-KY-OH | 7.70% |
| 188 | Duluth, MN-WI | 7.70% |
| 189 | Deltona-Daytona Beach-Ormond Beach, FL | 7.90% |
| 190 | Charleston, WV | 8.80% |
“Among the 48 communities examined nationwide, Boston and San Francisco metropolitan areas score the highest in their overall infrastructure to support active living, followed by Chicago, New York and Washington, D.C.,” said the report. “Indiana and Oklahoma each produce two of the bottom five active living communities: Fort Wayne, Indianapolis, Oklahoma City and Tulsa. Durham-Chapel Hill, North Carolina, has the fourth-lowest active living community ranking.”
The New York City and Boston metropolitan areas are the top two communities for both walkability and transit. Madison, Wisconsin, and Portland, Oregon, have the highest bike scores, while Minneapolis and Washington, D.C., have the highest park scores.
How can your community do the right thing? The report offers some examples … even in leading light Denver. And bicycling seems to be a thing:
- “Albert Lea, Minnesota, established more than 10 miles of bike lanes and new sidewalks and enhanced streets to support walking and biking. The city adopted policies to reduce tobacco use and started workplace programs to promote health and social interaction. Grocery stores, restaurants, schools and workplaces made changes to make healthy choices easier, and several restaurants added outdoor dining areas. These active living improvements helped Albert Lea increase its overall well-being score by 2.8 points from 2014 to 2016, significantly outpacing both the state and the nation.”
- “Marion, Iowa, requires consideration of pedestrian and cyclist needs in all street projects, and new developments must have sidewalks installed within five years. Guidelines integrate trees, green space and other natural features to make streets more walkable. The city’s “Complete Streets” policy has revitalized its historic Uptown district, redirecting cars from the area and creating a pedestrian-friendly atmosphere.”
- “Denver’s Department of Public Works coordinates a coalition to fund the Safe Routes to School (SRTS) program, constructing new trails to encourage children to walk or bike to school in safe environments. Residents of Denver’s Park Hill neighborhood trade community service for free refurbished bicycles. And Fort Collins, Colorado, has invested in at least 48 neighborhood parks and 35 miles of trail systems while boasting one of the best bicycle commuter rates in the nation.”
- “Eugene, Oregon, which has reduced its obesity rate since 2008, is home to well-planned and well-used cycling networks that include 28 miles of off-street paths, 78 miles of on-street bicycle lanes and four bicycle/pedestrian bridges spanning the Willamette River. Similar to Fort Collins, Eugene’s share of workers who commute by bicycle is one of the best rates in the nation among midsize cities; at 9 percent, it is well ahead of the national average, which is lower than 1 percent.”
- “In Chattanooga, Tennessee, the 2014-2015 obesity rate dropped by about four percentage points (from 28.5 percent to 24.6 percent) since 2008 — likely benefiting from the Grow Healthy Together Chattanooga (GHTC) partnership, which leverages Healthy Kids, Healthy Communities grant money to increase access to healthy fruits and vegetables, expand options for physical activity, and enhance infrastructure for safe movement of pedestrians and bicyclists.”
“There are tangible policies that communities can adopt to actively cultivate and improve residents’ well-being,” says Dan Buettner, National Geographic Fellow and founder of Healthways’ Blue Zones Project, in the report. His comments could just as easily apply to company wellness programs as to communities:
“Policies that nudge people into healthy activities — where it is easy to walk to the store, bike to a friend’s house, get access to fresh produce and be surrounded by healthy-minded, supportive friends — are ones that make the healthy choice the easy choice,” he said. “Sustained transformation depends on building an environment and establishing social policies that support and reinforce these programs.”